It’s been heart breaking watching the scene unfold in New York. As bad as it is, similar scenes are playing out now in Louisiana, Michigan and Texas. Those healthcare systems are being overwhelmed by a crush of cases coming through their doors. Yet in stark contrast there are parts of the country that are seeing minimal to mild activity of Covid-19 right now. They will likely see greater activity later but those peaks will not occur for several more weeks. Many states are projected to have minimal to no shortage of ICU or total beds, these include states like the Carolinas, Nebraska, Ohio, Vermont, Missouri, Oregon, and several others. I suggested previously that this extra capacity could be harnessed by the federal government by nationalizing the hospital supply chain and moving supplies around the country as needed. Taking advantage of existing supplies is the only way to deal with the current supply shortage because the federal stockpile does not have enough supplies of ventilators and PPE to help the entire country. While ventilators are being feverishly produced, they will not be produced in time to deal with the coming waves of patients in the next 1-2 months. The only way to manage this is to take a nationwide approach using the resources we have. It’s obvious that the President has no desire to do this, and seeing Governor Cuomo speaking the past few days he has come to this realization as well.
Governor Cuomo has thus sent out a call to workers from around the country stating that if they help New York, New York would come to their aid as well. Looking at the predicted surges in New York compared with other states around the country, this plan could work, other states could indeed come to the aid of the hardest hit states. However simply asking for their aid is not enough. The Governor needs to assure those other states that they can help New York without risking themselves in the process
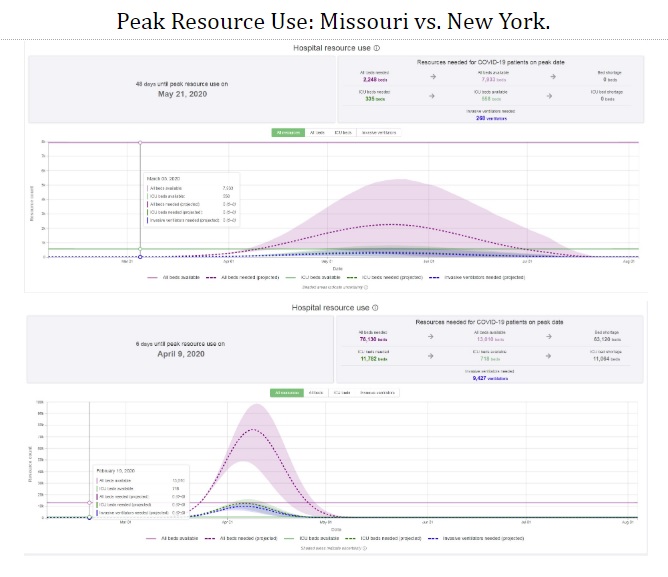
To my mind there are 2 basic hurdles to overcome for this to work. First is trust. How do other states know that the state(s) that they are helping will return their supplies and people when they are needed. To overcome this issue, the borrower state would need to have some sort of reciprocity agreement in place with the lending state. The reciprocity agreement would need to stipulate an expiration date on the provided assistance. That “Give Back” date should correspond to the projected surge date of the lending state. Looking at the figure above, a reciprocity agreement between Missouri and New York would require that New York would return any borrowed supplies and manpower by a certain date which would likely be around the last week of April. After that date, help would then move in the reverse direction. This return of resources would need to take place regardless of how bad things still were in New York, that way Missouri would be assured that it was not short changing it’s own people to help New York.
The second issue is manpower. Right now I work in one of those states that has not been hard hit but expects to have a surge of patients around the end of April and into May. While I would be happy to volunteer in a place that has an acute need right now, I would not go somewhere when my own home state is being overwhelmed. Additionally, before travelling somewhere else to volunteer, I would need to know that my job will still be here when I get back. Thus each state would have to have agreements in place not only to return supplies but also manpower. And they would have to stipulate that no health care worker will lose their employment when leaving their home to volunteer in the reciprocal state.
It’s clear that we do not have the time to build the supplies and hire the people that we need in the hardest hit areas. People will die from the disease, there’s little we can do about that now. But people will also die from lack of supplies, and people. That is inexcusable. The only way to save lives now is to help each other by pooling our collective resources. This is now a world war, World War C, it’s time we fought together.