The nurse practitioner on the other end of the phone call sounded stoic. She was calling from a rural hospital about 100 miles away from the large tertiary center ICU that I work in. She was doing her best to manage a COVID-19 patient, whose condition was declining rapidly.
“So you definitely can’t take this patient?” she asked.
“No” I said, “I’m so sorry, our ICU is full and we are no longer taking transfers” Her exasperated sigh made clear her disappointment. “Could you give me a consult?” she asked. “Of Course”, I replied. We walked through the patient again, she had done everything right. They had started the patient on all the right medications, she had placed the patient on their belly. We reviewed the ventilator settings. It was clear there was really not much else I would offer the patient, even if we had the beds. With COVID-19, sometimes you can do everything right, and still lose the battle. I wished her good luck and asked her to call back if she needed me.
Part of my job of being an ICU physician is fielding calls from surrounding rural hospitals, and I’ve been getting alot of calls like this.
It’s not that my hospital is full of covid patients, quite the contrary, most of the patients in hospitals right now are the run of the mill usual patients. But on a slow day in winter time, a hospital is probably going to be at 60 to 70 percent capacity. COVID has changed this. Now most of our hospitals’ extra capacity has been taken up by COVID patients, leaving practically no room to take care of patients from small rural hospitals.
While small and often understaffed, rural hospitals serve an outsized role in managing illness in rural areas that have limited access to health care. Unlike large urban centers which usually have critical care physicians managing ICU patients 24/7, these rural ICUs are often managed by hospitalists or nurse practitioners. These smaller hospitals often don’t have the staff or expertise to take care of extremely ill patients that require specialized care. They rely on having the safety net of urban tertiary care centers to help manage those patients.
Only now, that safety net is being ripped away. Without it, I’m not sure how they’ll manage these tremendously sick and complicated patients. Without the ability to transfer to a tertiary center more patients will need to be treated in rural centers than otherwise would have, and certainly that raises the likelihood that more patients will die in those centers than otherwise might have. At this point, our only cure is prevention. I am pessimistic that we will convince people to take precautions that they have, up until now, seemed unwilling to take. It would seem, therefore, that the coming vaccine is our best chance to stop this before it spirals out of control. Having worked with small rural hospitals in the past, I know that they are filled with dedicated professionals, as good as anywhere else in the country. But there’s only so much that they can take. Only time will tell how these hospitals handle the surge that is currently ongoing but I fear what will happen if it gets worse.
Deep Ramachandran, M.D. is a Pulmonary, Critical Care, Sleep Medicine physician, former CHEST Journal Social Media Editor, and co-Chair of ACCP Social Media Work Group. He blogs at Caduceusblog. He is on twitter @Caduceusblogger.




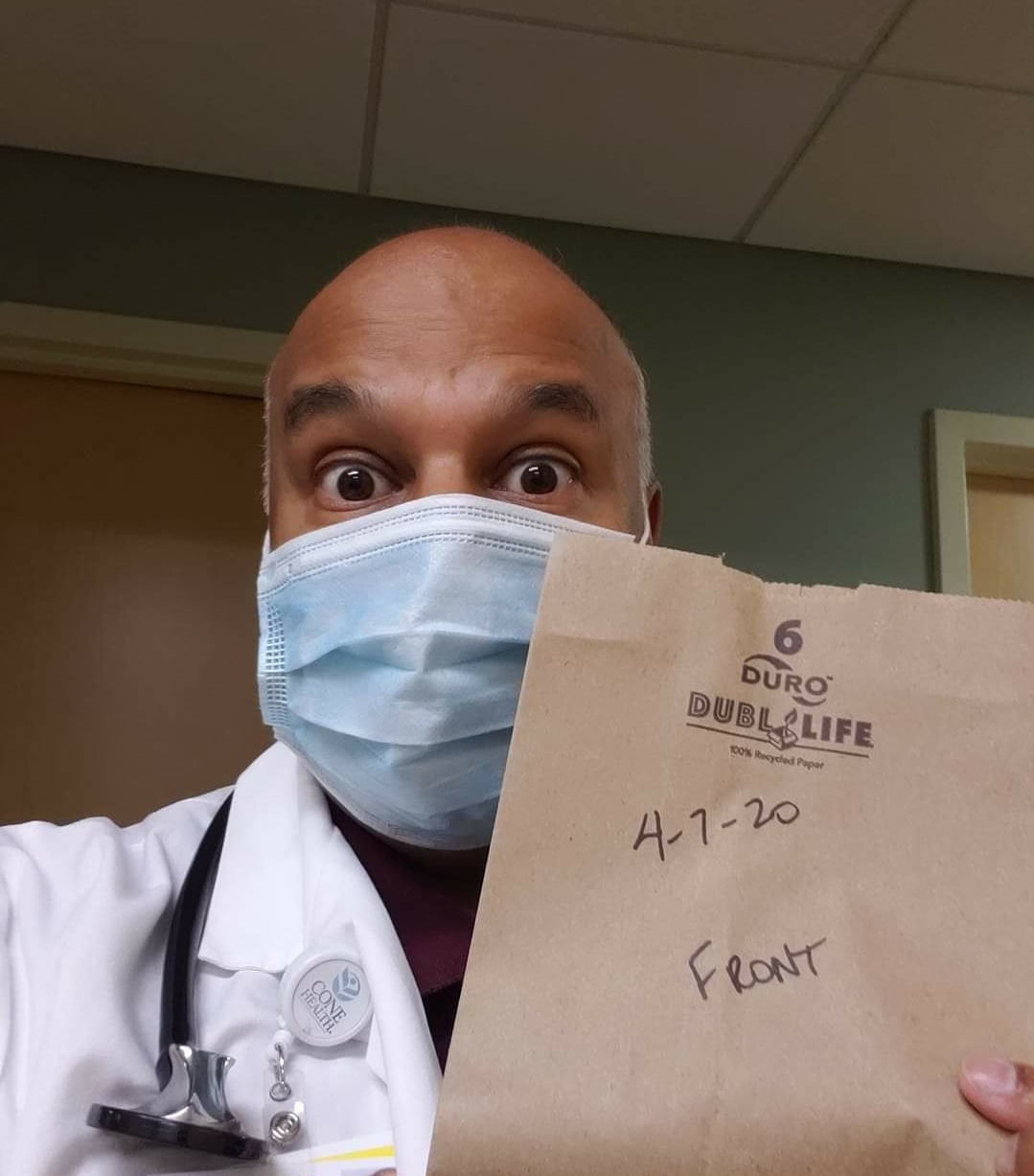 Look at this idiot.
Look at this idiot.
:strip_exif(true):strip_icc(true):no_upscale(true):quality(65)/arc-anglerfish-arc2-prod-gmg.s3.amazonaws.com/public/DF65YKARRNGKLGTOXGO27JG43M.jpg)