Disclaimer: The information contained in this post is up to date as of this writing. For the latest information, visit the CDC website on outbreak of ecigarette related vaping associated lung injury.
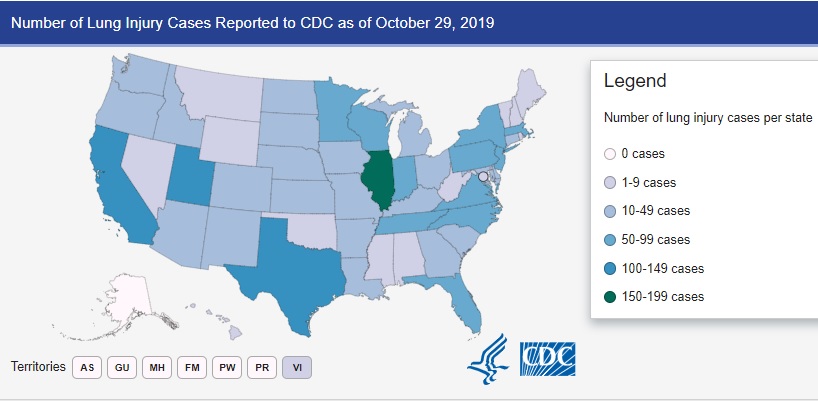
In September of 2019, the Wisconsin Department of Health Services and the Illinois Department of Public Health published the results of their investigation into a new clinical syndrome. This initial series involved a cluster of 53 cases of ecigarette vaping associated lung injury (EVALI). Since the initial study, the syndrome was found to be a national epidemic. Nearly 1900 people have been affected by vaping associated lung disease, there have been 37 deaths. Cases have been reported in all states except Alaska.
Case Definition: The first step in evaluating a new disease is determining the characteristics that make up that disease. In the case of EVALI, CDC has issued this publication to define cases of Confirmed or Probable EVALI for surveillance purposes. In general, this involves the presence of pulmonary infiltrates in the presence of vaping in the past 90 days and in the absence of infection or other plausible causes.
Presenting Symptoms: Interestingly, patients with EVALI appear to present in a number of ways. These include not only respiratory symptoms, but also with constitutional symptoms and gastrointestinal symptoms. In the initial series of patients in Wisconsin and Illinois, all patients had constitutional symptoms at presentation, most commonly subjective fever. Nearly all (98%) had respiratory symptoms at presentation, and 81% had gastrointestinal symptoms, of which nausea and vomiting were most common.
Exposures: While the particular vaping component that leads to EVALI is not yet known, there are a few common factors. 87% of patients with EVALI reported vaping THC, while only a small minority (<15%) reported vaping nicotine without any THC. However as many have pointed out, vaping THC in most states is illegal. In addition many of these patients are under the age of 18, thus it is reasonable to think that many who claimed not to have used THC use simply did not want to divulge that they had. So why would vaping THC lead to EVALI, when people have been smoking THC for decades? Vape liquids contain several chemicals including propylene glycol, terpenoids, cutting agents, and flavorings. These solvents are used to keep THC and other components, such as flavoring agents in solution. These solutions are prepared in different ways in back yards, garages, and back seats, often cut with unknown substances to reduce their cost. They are then sold as cartridges to people who use them in a variety of different vaping devices which themselves which may heat the fluid at different temperatures and for a different duration.
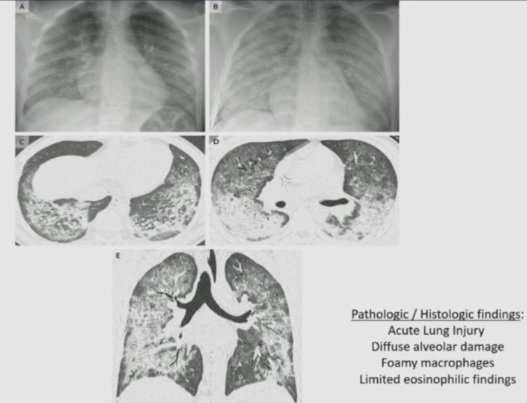
Radiologic Findings: Ct findings are often heterogenous in EVALI. They can include mild infiltrates to diffuse findings suggestive of ARDS/DAD.