Recently I read an article in the NY Times by Elisabeth Rosenthal. She’s the same author of the enlightening article “My doctor charged me $117,000 and all I got was this lousy hospital gown” That may not have been the exact title of the article. Continue reading “Why Doctors Don’t Like to Send You Test Results.”
Top 5 Ways That Television is Ruining Your Sleep.
As a sleep physician, I spend a lot of time educating patients about what sleep is and how it works. Sleep, as I often explain, is not simply the lack of being awake; anymore than landing a plane is simply the lack of flying. It’s becoming increasingly understood that sleep is an actively generated state, created by a series of neuro-hormonal changes which work in concert to nudge the brain into the sleep state. To stretch the plane analogy further, if being asleep were like the plane being on the ground, then falling asleep is like the act of landing the plane. And just like when you land a plane, there are a lot of variables that are involved. There are numerous events that must happen in succession, each affecting and triggering other events which ultimately induce the brain to sleep. A recent study demonstrates just how watching too much television can wreak havoc in this delicate process. Here’s just a few of the ways that television can ruin your sleep.
5. Watching television makes you go to bed later.
Television watching has steadily increased in our society, and its migration into our bedrooms marked a time when it began to disrupt our collective sleep and sleep habits. The most obvious effect that this might have is the most simple; we stay up later watching a program that has our attention. This few minutes a night may seem innocent enough. But our brains have a pre-determined amount of sleep they need to function well. When we miss that sleep we build up a “sleep debt” that can make us tired all of the time. Even if we catch up on a bit of sleep the next day, unless that sleep debt is paid back, the brain will still be fatigued.
4. Watching television alters your brain’s bedtime habits. Continue reading “Top 5 Ways That Television is Ruining Your Sleep.”
The Shocking Truth Behind “Shocking” Healthcare Social Media Statistics
As a regular follower of social media, I am keenly aware of changes in the healthcare landscape as it relates to social media. While there’s much talk about the impact of social media in healthcare, most of the action sits on the consumer side of the equation. Much of the medical world has to yet to tap into its potential. For most healthcare providers social media engagement amounts to little more than watching as others dip their feet, testing the waters. A few watch as they anticipate their own entry into the arena. Still many others watch with the expectation that the water would soon become bloody.
So its with a burlap full of salt that I read various healthcare social media stats promulgated in various infographics, twitter feeds, and blog posts celebrating Medicine 2.0 powered by social media. Collectively they hash and rehash a series of surprising statistics that aren’t exactly bogus, but aren’t exactly completely factual either.
A recent one caught my eye with the claim was that “53% of physicians practices have a facebook page”. This was curious to me, because as I read this in the physician lounge and took my own poll, the results was much closer to 5% than 50%. Continue reading “The Shocking Truth Behind “Shocking” Healthcare Social Media Statistics”
Top 5 CPAP Travel Tips from a Sleep Doctor and CPAP User.
Sleep Apnea is a condition that aflicts millions of people. There are 2 types of sleep apnea, central, and obstructive. Obstructive is by far the most common, and is usually what is referred to when people talk about “sleep apnea”. Obstructive sleep apnea occurs when, during sleep, the airway passages in the throat close and block the movement of air. Common symptoms are snoring, gasping during sleep, sleepiness during the day, and the overall feeling that your sleep was not restful. While we all may have a laugh recalling that uncle or grandpa that was “sawing logs” all night when they slept over, the truth is that sleep apnea can have profound negative effects on overall health. Sleep apnea has been linked with stroke, cardiovascular disease, hypertension, and is an important contributor to deaths and injuries due to traffic accidents. The most common and effective treatment for sleep apnea is the use of a CPAP (Continuous Positive Airway Pressure) device. As a sleep physician, and a CPAP user myself I know the importance of using your CPAP whenever you sleep, that includes during travel.
Whether I’m travelling across a state line or an equatorial line, whether the destination is medical education, or a mediterranean beach, my CPAP is along for the ride. Because of this, I’ve also run into pretty much every complication, problem, pitfall, morass, and quagmire that you can have when travelling with your CPAP. Thus I present to you, gleaned from both my experiences and those of my patients, my Top 5 tips for travelling with your CPAP.
- Bring Your CPAP With You!
This would seem obvious, but it’s not. Alot of people see their CPAP as an assistive device which they only need to use when they need it. But they really need to look at it for what it is: therapy. You take your hypertension and diabetes medicines with you when you travel, think of your CPAP the same way. Besides, if you’re travelling for business, you need to be sharp and focused. If you’re travelling for pleasure, well who wants to spend their hard earned vacation being tired and irritable? CPAP will help you get the most out your travels! Continue reading “Top 5 CPAP Travel Tips from a Sleep Doctor and CPAP User.”
Me and My A.E.D.
“Everyone should have BLS training. . . we’ll all be better off because of it” -Me.
I arrived at my designated gate at Chicago’s O’Hare Airport. The run there kept the adrenaline level up in my system, though the hubbub was now well behind. I pulled the crumpled boarding pass out of my pocket as I caught my breath. No that’s a hotel receipt. Check the other pocket, there it is, Zone 3, that can’t be that bad; I thought, there’s gotta be, what maybe 6 or 7 zones, right? “Welcome aboard American Airlines flight to Flint, Michigan” the gate attendant announced. We welcome our platinum medallion, gold medallion, silver medallion, bronze high-flyers, copper star club, as well as plastic fantastic, and purple star members, followed by zones one and two” The last of the passengers was already through the jetway. “Now boarding zone three, welcome aboard”.
After handing over my crumpled boarding pass for scanning, I made my down the jetway and onto what appeared to be a small but fairly packed little jet. Passengers on each side of the aisle eyed me as I walked past, a few noticed that my jeans were soaked from the knees down. Some caught the odor that trailed behind, a light of recognition igniting in their eyes as they realized what it was. Does he really smell like that? Is he the one that’s dragging that awful scent through this cabin?
6 hours earlier things had been going very differently for me. My colleagues and I had just given a well received talk at the annual Chest convention. I had reconnected with old friends that I hadn’t seen since training. I had just personally thanked Kevin Pho (of KevinMD fame) in the hotel coffee shop for giving our keynote address and getting our membership fired up about the future of medicine and social media. It was with this sense of excitement and renewed enthusiasm that I boarded my plane to catch a connection at O’Hare.
I also distinctly recall that, at the time, my pants were absolutely one-hundred percent completely dry. Continue reading “Me and My A.E.D.”
A Comedian Learns That He Has Sleep Apnea (Video)
Sleep Apnea is a serious condition that afflicts millions of people. The condition leads to reduced breathing during sleep which causes reduced oxygen to be delivered to the heart and brain. The condition may increase the risk of developing diabetes, hypertension, stroke, and depression. The reduced sleep quality can also lead to daytime sleepiness which can cause traffic and workplace accidents. In the video above comedian Jo Koy relates how he learned about the diagnosis of sleep apnea (he later got treated). Learn more about the disease and how you can get tested at SleepEducation.com.
Remember When We Used to Prescribe Inhaled Steroids for Asthma and COPD?
Press Release: Annual Conference of the Universal College of Chest Physicians October 2085; New Chicago, Mars.
The annual conference enjoyed another record attendance today as attendees flocked to Dr. Ramachandran III’rds keynote address reviewing exploits of physicians in the early part of the century. Dr. Ramachandran highlighted some key decisions and their consequences, such as the ACGME’s decree in 2032 that all residents should be swaddled before their scheduled hourly nap times. This of course led to the now infamous Great Hospital Apocalypses of 2033, 2034, and 2035.
Perhaps nearly as intriguing was the plight of inhaled corticosteroids for the treatment of respiratory diseases like asthma and COPD in the beginning of the 21st century. The period began with greater awareness and concern regarding the use of long acting beta agonist (LABA) bronchodilators such salmeterol. That risk was highlighted by findings published in the SMART trial (access through Chest archives here). There was increased concern regarding the potential harm caused by LABA which culminated in the placement of warnings on medications which contained LABA bronchodilators. These medications, experts said, were to be prescribed with extreme caution because of the possible increase in harm, particularly among children.
Scholars of the early 21st century thus highly recommended that asthmatics, especially children, be started on steroid inhalers before having to resort to using inhaled LABAs. Many also theorized that inhaled steroids had a protective effect when combined with LABA’s, possibly ameliorating their potential danger. Thus many at the time recommended a strategy of not using LABA inhalers at all, unless also simultaneously prescribing an inhaled steroid.
However, problems with this approach started to appear late in the first decade of the century. The TORCH study, a trial using combined inhaled LABA/inhaled steroids in adults with COPD suggested that there was an increased incidence of pneumonia among those treated with inhaled steroids. Early in the second decade a pivotal study then demonstrated that asthmatic children treated with inhaled steroids ended up being about half an inch shorter than they might have otherwise been (interestingly, a later study in 2035 correlated the reduced height with a statistically significant decrease in NBA dunking). Continue reading “Remember When We Used to Prescribe Inhaled Steroids for Asthma and COPD?”
How to Attend a Medical Conference Without Actually Being There.
Well, I’ve done it again. It seems that every time I try to make the early registration deadline for a conference, something seems to come up. One of the kids gets sick, a transmission breaks, I have a crazy week at work, you know, life.
Unlike previous years however, I’m very excited to say that I will be making it to the American College of Chest Physician’s annual scientific meeting at the end of October.
While I wasn’t able to make it to the conference every year, it turns out that I didn’t have to miss everything because I had a new and unique tool at my disposal. A tool that allowed me to catch a surprising amount of the action and actually obtain some of the benefits of the conference without actually being there: social media. Continue reading “How to Attend a Medical Conference Without Actually Being There.”
Why I Stopped Working with Express Scripts
Mail order pharmacies like Express Scripts and Medco have become increasingly prominent players in health care. But these companies are a lot more than simply mail order pharmacies, they are in fact a new generation of pharmacy benefit managers (PBM’s). PBM’s are essentially middle-men between insurance and pharmacy, with companies like Express Scripts merging the dual functions of a PBM and pharmacist into one. PBM’s manage and administer medication benefits for insurance companies. The largest insurance companies contract with them not only to manage the medication benefits of their clients (that would be you), but also to contain costs. Since insurance companies are not in the business of directly managing pharmacy services themselves, they contract with PBM’s to coordinate and manage their patients’ insurance benefits for them. If a PBM can do that at a lower cost, they save (make) money for themselves and the insurance company.
Mail order pharmacies are in a unique position to do this, as they don’t have to maintain brick-and-mortar outlets, and can use the mail to reduce costs . With such an advantage in cost containment, mail order PBM’s are quickly pushing traditional brick and mortar outfits to the periphery (remember Netflix vs. Blockbuster?). Mail order pharmacies are thus becoming giants in this industry. In 2012, Express Scripts completed a $29 billion acquisition of Medco, to create the country’s largest PBM, a publicly traded company with $100 billion in annual revenue.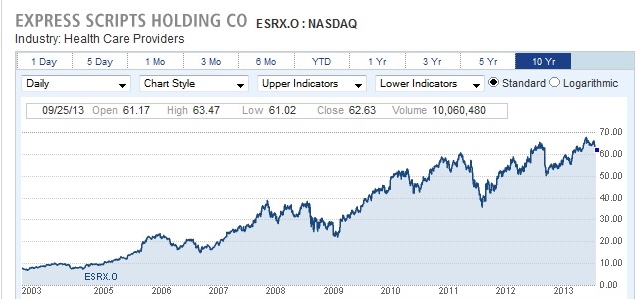 Continue reading “Why I Stopped Working with Express Scripts”
Continue reading “Why I Stopped Working with Express Scripts”
Smartphone App Allows COPD Patients to Individualize Their Care.
Health-care technology advocates have long been preaching about the potential of smartphones and other types of disruptive technology to improve health-care delivery. We in organized medicine have been slow to answer the call. Studies that showcase the ability of these tools in major medical journals are rare. However, in a recent issue of CHEST, we see a welcome addition to the medical literature.
In this study, researchers taught patients with COPD to create daily symptom diaries on smartphones (BlackBerry 8700s). The results were uploaded to a research server and the program alerted staff when certain predetermined criteria were met. Using the data, researchers were able to accurately and quickly identify patients who were having an exacerbation of their COPD. They were also able to collect data on both the timing and length of the exacerbation.
This has exciting implications. Perhaps this kind of patient centered data could be used to identify patients with severe symptoms and prevent hospitalizations, or to serve as a measure of response in clinical trials to various interterventions. The possible applications are numerous.
Though there is one aspect of this study that, as a tech geek, leaves me ambivalent. Should I be excited that even an obsolete smartphone could prove to be so useful? Or depressed that even an obsolete smartphone is so far ahead of current medical technology?
This article is also posted at the ACCP Thought Leaders Blog.
